Prevention
Modern medicine is increasingly transitioning towards preventive care. This shift towards prevention has also been observed in breast cancer care in recent years, particularly with the discovery of the BRCA gene. Subsequently, multiple genes and risk factors have been identified. Depending on these factors, a personalized screening strategy can be chosen. Therefore, it is crucial to understand these genetic and risk factors.
Diagnosis
I was diagnosed with cancer ... This website serves as a portal designed to assist you and your loved ones in accessing personal information and finding solutions to your concerns.
The primary goal of this website is to offer guidance and support to patients as they navigate their journey toward recovery and improved quality of life. The "Diagnosis" section of our website is divided into two main categories. Firstly, under "Anatomy and Physiology," we provide fundamental knowledge about the breast. Secondly, in the "Tumors and Disorders" section, we delve deeper into various breast-related conditions.
Moreover, we aim to provide information to women who may be concerned about potential breast issues but are hesitant to seek immediate medical advice. Knowledge and information can often offer immediate reassurance if a woman is able to identify the issue herself and determine that no specific treatment is necessary. Conversely, we also strive to educate women who have received a diagnosis of a serious breast condition, such as breast cancer, and wish to approach their doctor well-informed and prepared.
Treatment
The treatment for breast cancer should immediately include a discussion about reconstruction. Our foundation has no greater goal than to raise awareness of this among patients and oncological surgeons. By making an informed decision beforehand, we avoid closing off options for later reconstruction while still considering the oncological aspect. Of course, survival is paramount, and the decision of the oncologic surgeon will always take precedence.
The "Reconstruction or not?" page contains all the information you can expect during an initial consultation before undergoing tumor removal. This page is comprehensive, and your plastic surgeon will only provide information relevant to your situation.
"Removing the tumor" details the surgical procedure itself. This is the most crucial operation because effective tumor removal remains paramount. We guide you through the various methods of removal, a decision often made by a multidisciplinary team comprising oncologists, radiologists, pathologists, radiotherapists, breast nurses, gynecologists, oncological surgeons, and plastic surgeons.
The "Breast Reconstruction" section includes information and illustrations of the different reconstruction options along with corresponding steps.
Revalidation
Those treated for cancer often need a long period to recover.
Cancer is a radical illness with a heavy treatment. Often, people have to deal with psychosocial and/or physical problems afterwards, such as stress, anxiety, extreme fatigue, painful joints, reduced fitness, lymphedema... This can have a major impact on general well-being.
There are rehabilitation programmes offered by most hospitals. We cover some of the major topics here.
Quality of life
Quality of life is a key factor in coping with breast cancer. Therefore, it is important to find coping mechanisms that work, which will be different from patient to patient. For some, it may be finding enjoyment in activities they engaged in prior to diagnosis, taking time for appreciating life and expressing gratitude, volunteering, physical exercise... Of prime importance, studies have shown that accepting the disease as a part of one’s life is a key to effective coping, as well as focusing on mental strength to allow the patient to move on with life. In this section we are addressing some topics that patients experience during and after treatment and we are providing information to address them.
Removing the tumor
Removing as much as possible of the mass of the malignant tumor is the basis of further treatment and determines the prognosis of this disease.
Although the tumor and its offshoots must be completely removed, it is not always necessary to completely remove the mammary gland.
Introduction
Depending on the size of the tumor, the size of the breast, the location of the tumor, the possible presence of other tumors, the type of tumor and the preferences of the patient, the following types of resection can occur:
a tumoractomy: the removal of the tumor with a certain safety margin
a segmentectomy: the removal of a segment of the breast
a mastectomy: the complete removal of the mamary gland
You will find more information about these procedures on the relevant pages.
This can be combined with a sentinel gland biopsy of the axillary glands or a partial surgical removal of the axillary glands.
If you would like to have some more specialized information about how we approach breast surgery in general, you can read about the "3-step principle".
The 3-step principle
The 3-step principle of breast analysis was developed to help describe and deal with complex deformities of the female breast. It divides the breast into 3 simple anatomical features; the footprint, the conus and the skin envelope.
Applying the 3-step principle greatly simplifies surgical planning and management.
1. The footprint
The footprint is the outline of the breast base on the chest wall and is the interface of the posterior surface of the breast with the thoracic cavity. The footprint forms the foundation of the overlying three-dimensional structure of the breast (fig. 1).
The footprint can easily be seen at the end of a mastectomy, if the overlying skin is retracted, exposing the serratus anterior and pectoral muscles.
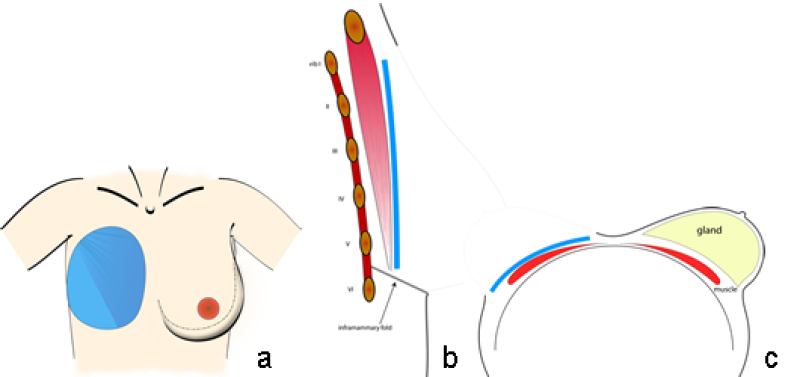
Fig. 1: Typical size and position of the breast footprint on the chest wall on a frontal (a) sagittal standing (b) and an axial supine view (c).
2. The conus
The conus refers to the three dimensional shape, projection and volume of the breast. It is normally formed by the mammary gland and sits anterior to the footprint of the breast (fig. 2). Each conus has a specific volume and yet its composition is different in every individual woman. The base of the conus corresponds to, or is slightly smaller than, the breast footprint. In a standing position, there is a gradual transition of the chest wall into the upper and medial aspects of the female breast. The infraclavicular area is typically flat or even slightly concave. This transition at the lateral and inferior part of a normal breast is sharper and may even reach 180° at the lower border of hypertrophic or severely ptotic breasts. The conus typically has lower lateral fullness, a maximum projection at the level of the nipple-areolar complex just lateral to the mid-clavicular line and a varying degree of ptosis.
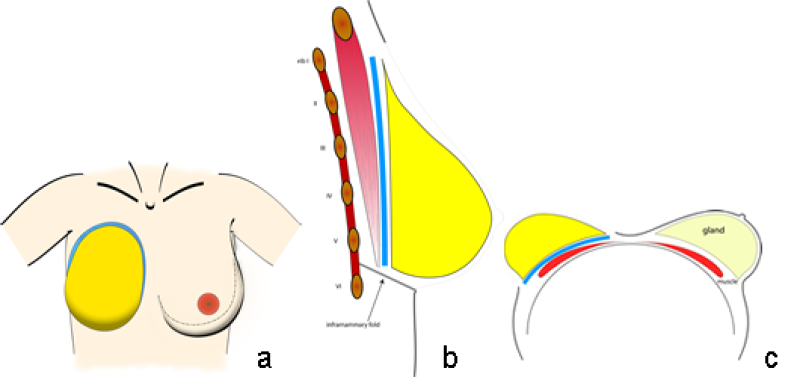
Fig. 2: Typical size and position of the footprint (blue) and the conus (yellow) of the breast on the chest wall in a frontal (a) sagittal standing (b) and an axial supine view (c).
3. The skin envelope
The skin envelope is the overlying skin and subcutaneous fat of the breast (fig. 3). Normally the skin envelope functions like a well-fitting brassiere, holding the conus in position and aiding projection.
The interface between the skin envelope and the conus can play an important role in breast shape. Scarring, due to surgery or radiotherapy, can tighten the envelope, while stretching of Cooper’s ligament or the superficial layer of the superficial fascia can loosen this envelope.
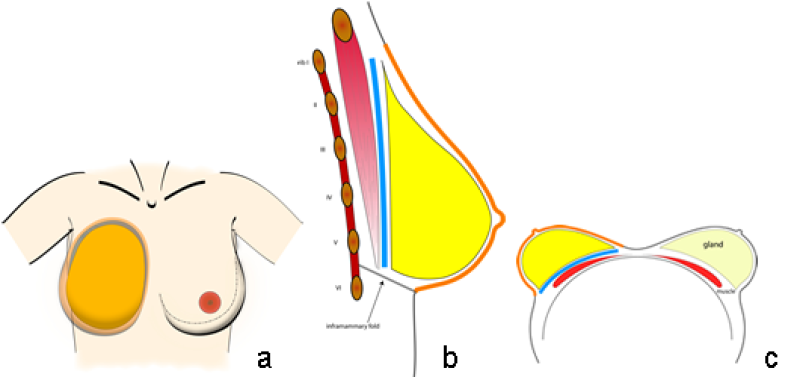
Fig. 3: Typical size and position of the footprint (blue), the conus (yellow) and the skin envelope (orange) of the breast on the chest wall in a frontal (a) sagittal standing (b) and an axial supine view (c).
The nipple-areolar complex (NAC) is also a component of the skin envelope. It contributes to the overall aesthetic appearance of the breast, by highlighting the point of maximal anterior-posterior projection, along either the vertical meridian line or slightly lateral to it (fig. 4). An attractive areola is pigmented, has a conical shape and is a smooth continuation of the natural contour of the skin envelope of the breast. The nipple protrudes above the areola. Nipple-areolar complex color and nipple dimensions are subject to wide variation and individual preference.
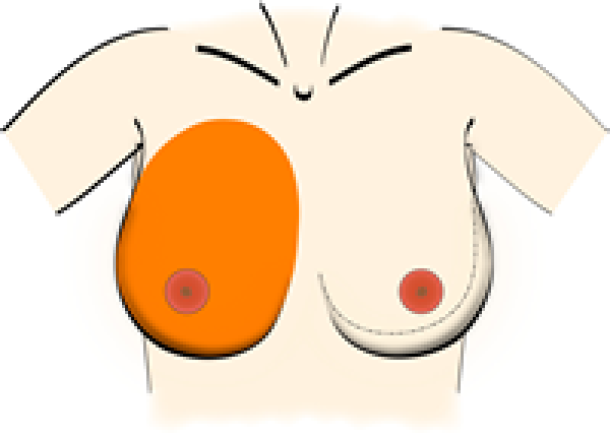
Fig. 4: The nipple-areolar complex (NAC) sits at the point of maximal anterior-posterior projection of the breast, either along the vertical meridian line or just slightly lateral to it.
The final breast shape is not determined independently by the footprint, the conus or the skin envelope. It is the interaction of these 3 elements that contributes to the maintenance of a pleasing, natural-looking breast over time.
References
Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Blondeel PN, Hijjawi J, Depypere H, Roche N, Van Landuyt K. Plast Reconstr Surg. 2009 Feb;123(2):455-62.
Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part II–Breast reconstruction after total mastectomy. Blondeel PN, Hijjawi J, Depypere H, Roche N, Van Landuyt K. Plast Reconstr Surg. 2009 Mar;123(3):794-805.
Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part III–reconstruction following breast conservative treatment. Blondeel PN, Hijjawi J, Depypere H, Roche N, Van Landuyt K. Plast Reconstr Surg. 2009 Jul;124(1):28-38.
Discussion. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part III–reconstruction following breast conservative treatment. Nahabedian MY. Plast Reconstr Surg. 2009 Jul;124(1):39-40.
Discussion. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part III–reconstruction following breast conservative treatment. Hammond DC. Plast Reconstr Surg. 2009 Jul;124(1):41-2.
Discussion. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part IV–aesthetic breast surgery. Hammond DC. Plast Reconstr Surg. 2009 Aug;124(2):385-6.
Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part IV–aesthetic breast surgery. Blondeel PN, Hijjawi J, Depypere H, Roche N, Van Landuyt K. Plast Reconstr Surg. 2009 Aug;124(2):372-82.
Discussion. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part IV–aesthetic breast surgery. Nahabedian MY. Plast Reconstr Surg. 2009 Aug;124(2):383-4.
Tumorectomy
A benign tumor does not have the ability to spread to distant organs and therefore can be completely excised. As it grows, it pushes away breast tissue and usually has a clear boundary around it. The goal of surgery is to remove the tumour but none of the surrounding normal breast tissue.
Removing a malignant tumor is different. A malignant tumor has fine offshoots that grow in all directions. These resemble the tentacles of an octopus. This boundary is often difficult to determine but it is essential to completely remove a malignant tumor. To ensure that the tumor and all its possible extensions are excised, a wide margin of surrounding normal tissue has to be removed.
The excised tissue is then examined under a microscope to check that all the offshoots have been removed. The edge of the removed breast tissue specimen is called the ‘tumor free resection zone’ or ‘tumor-free margin’.
Before undertaking a surgical procedure to remove the tumor, the exact nature and extent of the tumor should be determined to help plan surgery and fully inform the patient. All the possible alternatives to treat the tumor should be explained.
The removal of a breast tumor depends on its nature . The difference between a benign lesion and a breast cancer can be determined by physical examination and imaging of the tumor by mammography and ultrasound.
Ultimately, in all patients, confirmation of the diagnosis should be obtained before surgery by removing a small portion of the tumor and sending it for microscopic examination.
This is mostly done by needle biopsy:
With fine needle aspiration, cells that are aspirated can be examined under the microscope.
The most accurate method of histological diagnosis is a cylindrical biopsy. This is harvested using a slightly larger needle. This enables a more detailed microscopic examination and therefore accurate diagnosis.
A mammotome is a vacuum assisted breast biopsy device that uses X-ray, ultrasound or MRI to perform a small breast biopsy. A mammotome biopsy can be done under local anesthesia and removes only a small amount of healthy tissue.
If the tumor is detected early and is small, only the tumor itself and a limited rim of healthy tissue of the breast may need to be removed. This surgical procedure is called a tumorectomy (fig. 1).

figure 1a: status after biopsy (fresh scar around the areola) of a tumor recurrence after a wide tumorectomy in the lower-inner quadrant of the right breast. Shape and volume asymmetry are visible but not grossly disturbing.

figure 1b: status after tumorectomy in the upper-inner quadrant of the right breast. Shape and volume asymmetry are visible but not grossly disturbing.
Incisions can be made over the tumor or at more concealed locations like the edge of the areola or within the crease below the breast (figure 2). After removal of the tumor, it will be examined histologically.
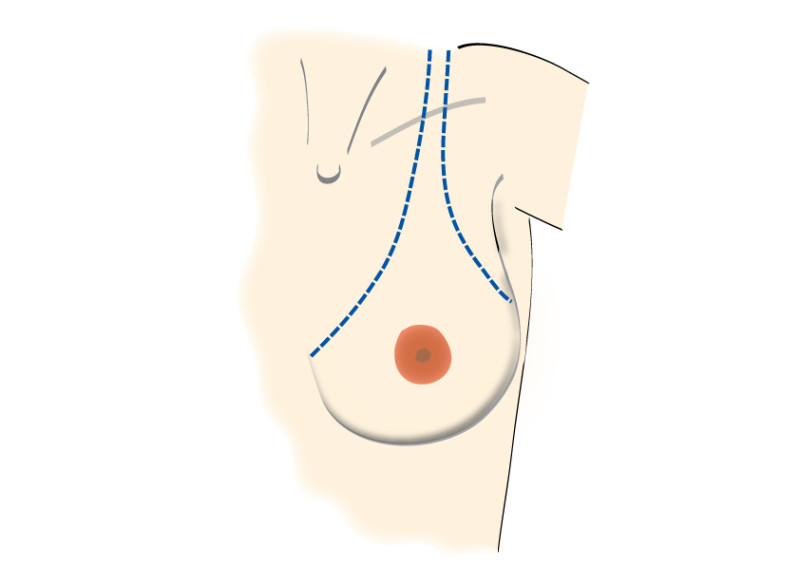
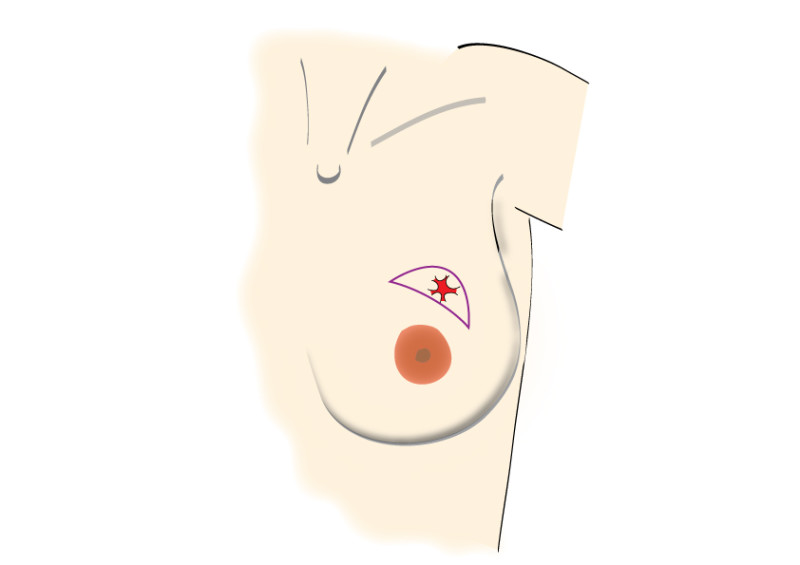
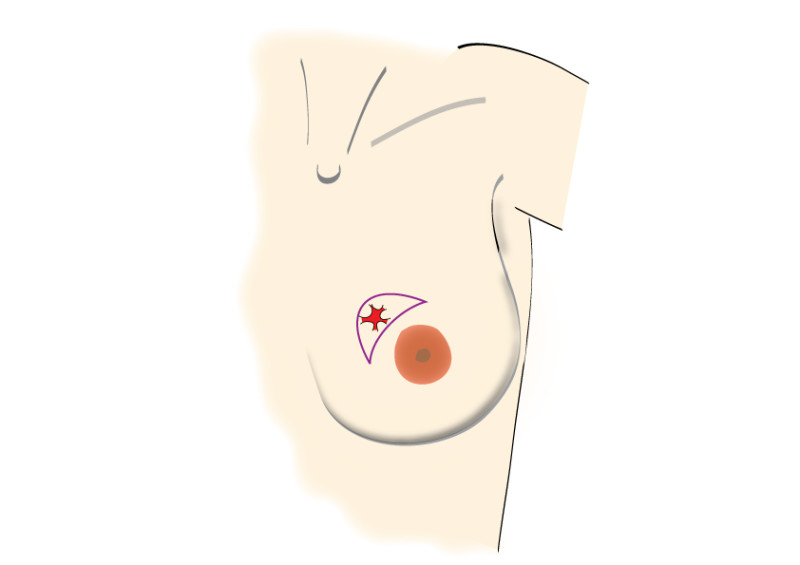
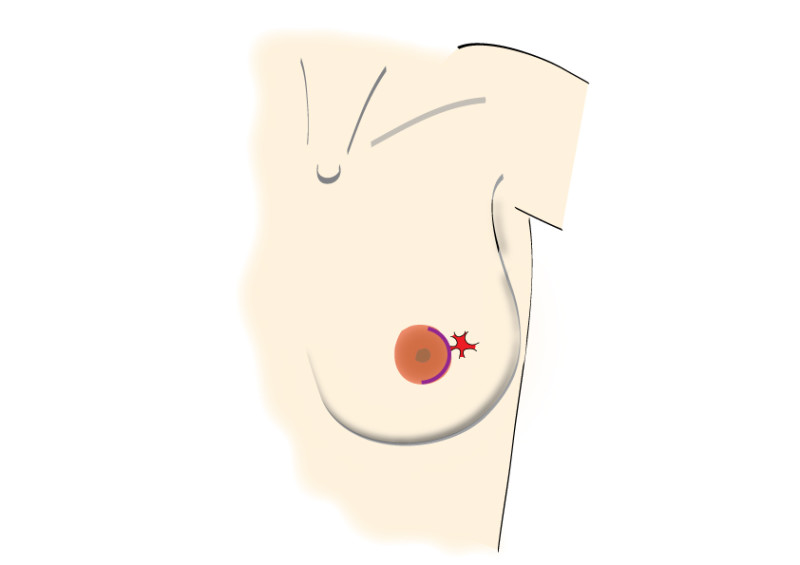
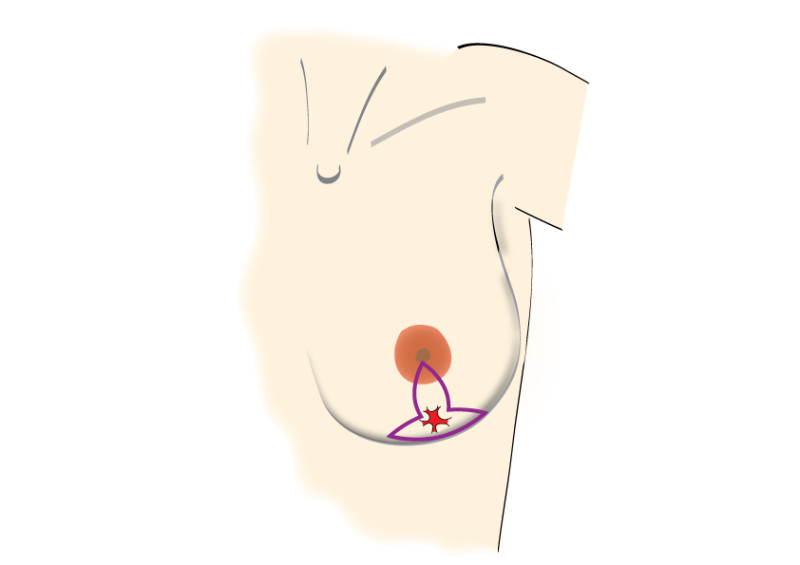
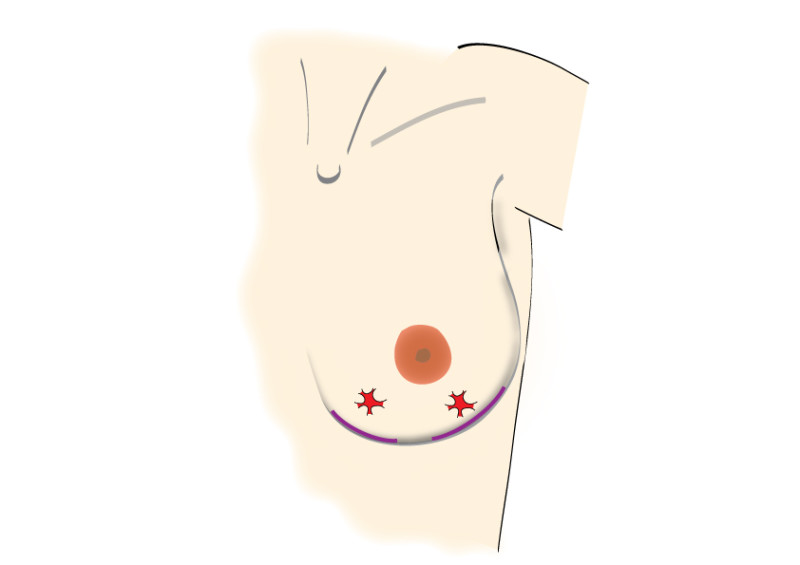
Fig. 2: possible incisions in the breast depending on size and location of the tumor. It is very important to position the incisions within the limits of the bra-line (first drawing).
Using mammographic screening, which is supported by most European Countries, small tumors that cannot be felt from outside can be detected. These tumors are often not palpable and so their removal is performed by needle localisation. Pre-operatively, a wire is placed by a radiologist to identify the site of the tumor (fig. 3a). At surgery, the wire is traced and the tissue at the tip of the wire is excised. The tissue with wire in situ are then sent back to the radiologist, while the patient is kept under anesthesia. The radiologist takes an X-ray to confirm that the correct area has been removed (fig. 3b).
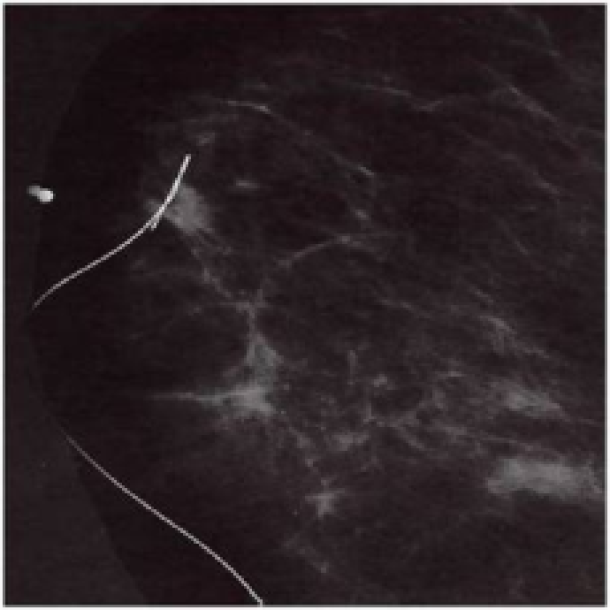
Figure 3a: mammogram with needle localization of a non palpable tumor.
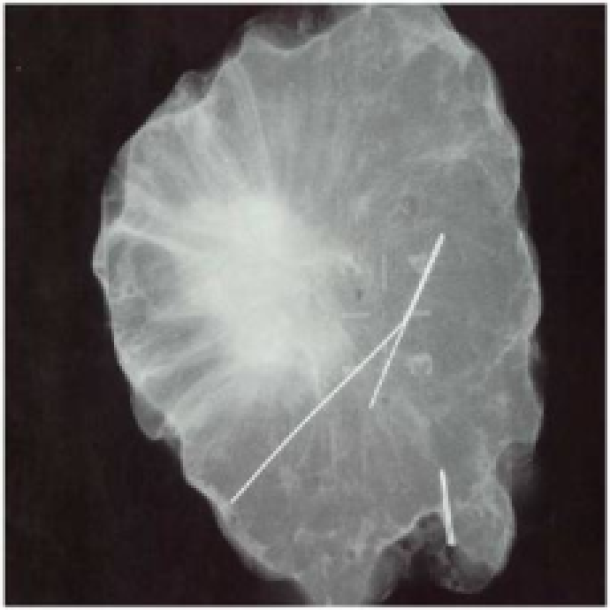
Figure 3b: X-ray of the same tumor after resection of both the tumor and wire.
If the wire indicates that the tumor is in the center specimen, one can be certain that it has been removed with a sufficient tumor-free margin. If the tumor is however close to one edge of the specimen, some additional breast tissue can be removed (wider excision) while the patient remains asleep.
If, after tumorectomy, the aesthetic appearance of the breast is affected, breast reconstruction may be indicated. Today small defects can easily be corrected by simple lipofilling. The different methods of breast reconstruction are discussed in other areas of this website.
References
Consensus conference on breast conservation. Schwartz GF, Veronesi U, Clough KB, Dixon JM, Fentiman IS, Heywang-Köbrunner SH, Holland R, Hughes KS, Mansel RE, Margolese R, Mendelson EB, Olivotto IA, Palazzo JP, Solin LJ; Consensus Conference Committee. J Am Coll Surg. 2006 Aug;203(2):198-207.
Outcome of breast-conserving therapy in the Tokyo Women’s Medical University Breast Cancer Society experience. Karasawa K, Obara T, Shimizu T, Haga S, Okamoto T, Ito Y, Kamio T, Kimura T, Kameoka S, Mitsuhashi N, Nishikawa T, Aiba M, Izuo M. Breast Cancer. 2003;10(4):341-8.
Integration of plastic surgery in the course of breast-conserving surgery for cancer to improve cosmetic results and radicality of tumor excision. Petit JY, Rietjens M, Garusi C, Greuze M, Perry C. Recent Results Cancer Res. 1998;152:202-11.
Ten year results of a randomised trial comparing two conservative treatment strategies for small size breast cancer. Mariani L, Salvadori B, Marubini E, Conti AR, Rovini D, Cusumano F, Rosolin T, Andreola S, Zucali R, Rilke F, Veronesi U. Eur J Cancer. 1998 Jul;34(8):1156-62.
Breast-conserving treatment: controversies and consensus. Noguchi M, Kinne DW, Miyazaki I. J Surg Oncol. 1996 Jul;62(3):228-34.
Controversies in the local management of invasive and non-invasive breast cancer. Page DL, Johnson JE. Cancer Lett. 1995 Mar 23;90(1):91-6.
Segmentectomy and quadrantectomy as part of breast conserving
Removing larger malignant tumors can be performed in different ways; either the breast is removed completely (mastectomy) or only the affected part is widely excised (breast-conserving surgery).
Whether or not breast-conserving surgery is possible depends on several factors. Recent studies demonstrate however that even with a sufficient tumor-free margin, breast-conserving surgery combined with radiotherapy, may result in a slight increased risk for local recurrence compared to a mastectomy. Long-term survival was similar in both groups.
The skin incision is performed over the tumor and the tumor is removed with a cuff of surrounding healthy breast tissue. Certainly with larger tumors, there is always a small chance that the tumor has not been completely removed. The excised part is therefore analyzed by a histopathologist. This doctor fixes the tissue, cuts it into thin slices, stains it and studies the specimens under a microscope to check if the tissue edges are tumor free. This process usually takes at least one week.
A second procedure may be needed if the tumor is not completely removed. Once the tumor has been completely excised, the remaining breast needs to be irradiated. This is done to eradicate any undiscoverable microscopic satellite lesions that could possibly be growing in the remaining breast gland tissue. The combination of surgery and radiotherapy can result into variable degrees of deformation of the remaining breast according to the sensitivity of each person to irradiation.

Figure 1: Breast conservative surgery: examples of breast deformation after segmentectomy and variable reactions to post-operative radiation therapy.
If the lesion is large or if the breast is small then the amount of tissue that needs to be removed may be relatively large in comparison to the volume of the breast. In this case we will use the terms segmentectomy (removing a segment of the breast, fig. 1) or quadrantectomy (removing one quarter of the breast, fig. 2) . In such instances, corrective surgery should be considered in a later phase as the defect can leave some important irregularities in the shape of the breast, specially when combined with radiotherapy (which almost always will be the case).

Figure 2: Breast conservative surgery: examples of breast deformation after quadrantectomy and variable reactions to post-operative radiation therapy.
Reconstructive options should be offered and discussed before performing ablative surgery, preferably with a plastic surgeon specialized in reconstructive breast surgery. The different methods of breast reconstruction are discussed in other areas of this website. Depending on the relative proportion of breast that has been removed, in general, different reconstructive options are proposed.
The table with the algorithm below summarizes the general approach of defects of the breast. Be aware that other or different decisions may be taken for every individual, depending on local tissue conditions. Options need to be discussed with your reconstructive surgeon.
Relative amount of breast gland removal | Reconstructive technique |
< 1/8 of the total breast volume | Re-arragnement of the remaining gland |
Lipofilling | |
> 1/8 and < 3/8 of the total breast volume | Loco-regional pedicled skin flaps |
Lipofilling | |
> 3/8 of the total breast volume | Removal of the remaining gland |
Full breast reconstruction with free flaps or implants |
References
Different annual recurrence pattern between lumpectomy and mastectomy: implication for breast cancer surveillance after breast-conserving surgery. Yu KD, Li S, Shao ZM. Oncologist. 2011;16(8):1101-10. Epub 2011 Jun 16.
Trends in the surgical treatment of breast cancer. Morrow M. Breast J. 2010 Sep-Oct;16 Suppl 1:S17-9.
Modified Benelli approach for superior segmentectomy: a feasible oncoplastic approach. Lanitis S, Hadjiminas DJ, Sgourakis G, Al Mufti R, Karaliotas C. Plast Reconstr Surg. 2010 Oct;126(4):195e-197e.
Quandrantectomy versus lumpectomy for small size breast cancer. Veronesi U, Volterrani F, Luini A, Saccozzi R, Del Vecchio M, Zucali R et al. Eur J Cancer 2009; 26:671–673.
Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Anderson BO, Masetti R, Silverstein MJ. Lancet Oncol. 2005 Mar;6(3):145-57.
Lumpectomy plus tamoxifen with or without irradiation in women 70 years of age or older with early breast cancer. Hughes KS, Schnaper LA, Berry D, Cirrincione C, McCormick B, Shank B et al. N Engl J Med 2004; 351:971–977.
Better cosmetic results and comparable quality of life after skin-sparing mastectomy and immediate autologous breast reconstruction compared to breast conservative treatment. Cocquyt VF, Blondeel PN, Depypere HT, Van De Sijpe KA, Daems KK, Monstrey SJ, Van Belle SJ. Br J Plast Surg. 2003 Jul;56(5):462-70. Breast tumor recurrence following lumpectomy with and without breast irradiation: an overview of recent NSABP findings. Fisher B, Wickerham DL, Deutsch M, Anderson S, Redmond C, Fisher ER. Semin Surg Oncol. 1992 May-Jun;8(3):153-60. Veronesi U, Salvadori B, Luini A, et al.
Conservative treatment of early breast cancer: Long-term results of 1232 cases treated with Quadrantectomy, Axillary dissection, and radiotherapy. Ann Surg. 1990;211:250-259.
Mastectomy
A mastectomy should be performed when:
The tumor is large compared to the overall size of the breast. When the tumor is very large, chemotherapy can be administered pre-operatively to reduce its size. When the tumor responds to the chemotherapy, breast-conserving surgery may be possible. As a general rule, if more than 1/8 of the breast volume needs to be excised, the aesthetic result after treatment (breast conserving surgery and radiotherapy) will be quite poor, mainly due to the effects of the radiotherapy.
Prophylactic mastectomy (see below): The breast is removed before a cancer occurs. This is recommended for women with a strong genetic predisposition to breast cancer.
Multifocal tumors: when two or more malignant tumors are present in different quadrants of the same breast; or if a malignant tumor is surrounded by satellite lesions; or there is a large area of dysplastic tissue; or there are multiple areas of carcinoma in situ.
Women who have previously been irradiated. This may be the case in patients who have certain forms of leukemia or who have previously undergone breast-conserving surgery combined with radiotherapy and now are confronted with a recurrence.
Severe comorbidities: in elderly women or women who have severe heart or blood vessel disease, severe lung disease or a combination of the above, it is prudent to perform a short procedure. Particularly if the entire breast is removed, one can be sure that no additional surgery will be necessary.
Tumors that have eroded through the skin.
A woman who choses to have her breast completely removed.
In many breast cancer patients, unfortunately, a mastectomy is still required. Fortunately we have moved away from the conventional radical mastectomy and in the majority of cases a modified radical mastectomy is performed.
Even less radical surgery can be offered to patients, depending on their tumor:
Skin sparing mastectomy involves resection of the nipple-areola complex together with the underlying mammary gland but preservation of the skin envelope. Often, the entire gland can be removed through a periareolar incision but if necessary, a short vertical incision can be added in the mid-areolar line.
Areola sparing mastectomy preserves the entire skin envelope and areola but sacrifices the nipple. A vertical incision is made at the mid-areolar line and continued to approximately 1 cm above the infra-mammary fold, to protect this anatomically important structure. The nipple is then removed together with the underlying mammary gland (fig 1.).
In many prophylactic mastectomy cases, a subcutaneous mastectomy is performed, retaining the entire nipple-areola complex. Incisions can be made in the mid-areolar line, in the inframammary fold or through any type of breast reduction/mastopexy pattern incision.
Type of mastectomy or partial gland removal | Anatomical structure that is removed | ||||||
| Breast gland | Nipple | Areola | Breast skin | Axillary lymph nodes | Pectoralis muscle | sternal lymph nodes |
Extended Radical Mastectomy | X | X | X | X | X | X | X |
Radical Mastectomy (Halsted) | X | X | X | X | X | X |
|
Modified Radical Mastectomy (Madden & Patey) | X | X | X | X | X |
|
|
Simple Mastectomy | X | X | X | X |
|
|
|
Skin Sparing Mastectomy | X | X | X |
|
|
|
|
Areola Sparing Mastectomy | X | X |
|
|
|
|
|
Subcutaneous Mastectomy | X |
|
|
|
|
|
|
Segmentectomy, Quadrantectomy, | partial |
|
| +/- |
|
|
|
Tumortectomy | small part |
|
|
|
|
|
|
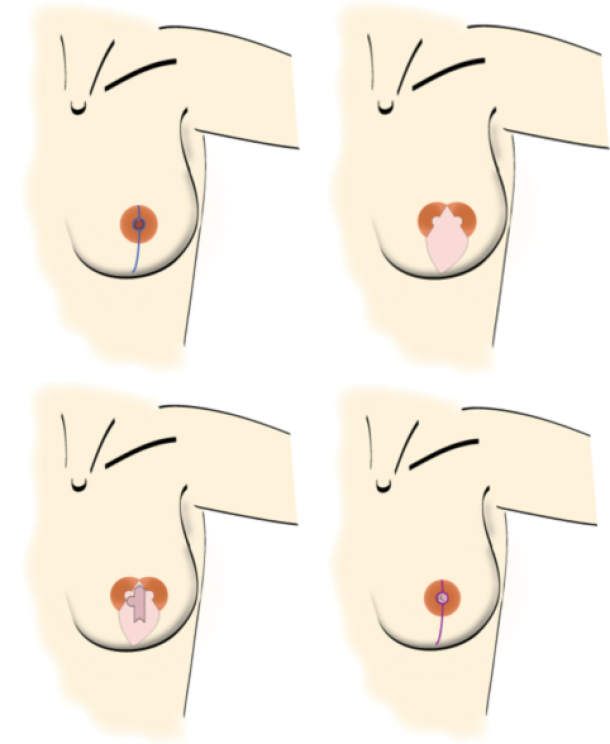
fig.1: Steps in an areola-sparing mastectomy. (a) skin incision for an areola-sparing mastectomy, splitting the areola into two halves and extending to about 1 cm above the inframammary fold; the nipple will be removed. (b) an elliptical skin island of the free flap is fit within the mastectomy skin edges. (c) this skin is used in the second procedure to reconstruct the nipple by means of a modified C-V flap technique. (d) after removal of redundant free flap skin, the wound edges are closed to restore the round shape of the areola and finish with a vertical infra-areolar scar. The new nipple still needs to be pigmented by tattooing during a short third session.
Depending on the patients’ wishes and the breast size and shape, a skin-sparing mastectomy can be combined with either reduction of the skin envelope or a breast lift procedure.
To achieve the best aesthetic result in an immediate reconstruction, it is important to preserve the inframammary fold, the pectoral muscles and the skin envelope during the mastectomy. If any of these anatomical structures are disrupted, they should be repaired before introducing an implant or autologous tissue.
In particular, if there is a deficiency in the skin envelope, then this needs to be addressed. In an immediate autologous reconstruction, the skin can be replaced with skin from the flap. In the case of implant based reconstruction, the extra skin has to be recruited by gradual tissue expansion.
When a patient presents requesting a delayed breast reconstruction, the surgeon has to assess the level of post-ablative damage and the effect of any previous radiotherapy on the chest wall. The more aggressive the initial ablative surgery, the higher the dose of radiotherapy administered (or sensitivity to the radiotherapy), the higher number and type of previous reconstructive attempts and the absence of the nipple-areolar complex, all make the reconstructive procedure more complex and adversely influence the final result.
Examples of different types of mastectomies:

Figure above: schematic drawing and clinical example of a patient who has undergone a modified radical mastectomy without reconstruction.
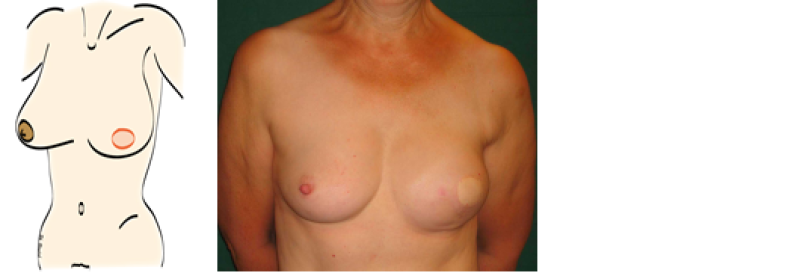
Figure above: schematic drawing and clinical example of a patient after a skin sparing mastectomy and an immediate autologous breast reconstruction. A nipple reconstruction still needs to be performed.
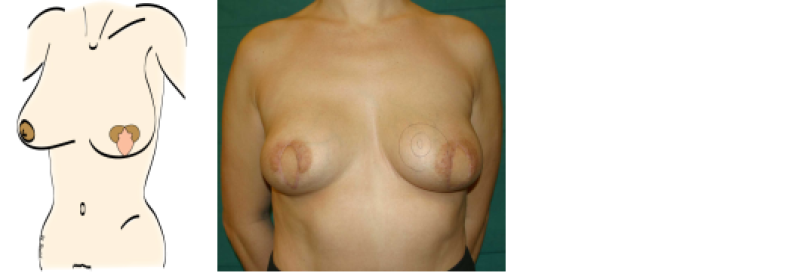
Figure above: schematic drawing and clinical example of a patient who underwent an areola-sparing mastectomy and an immediate autologous breast reconstruction.

Figure above: schematic drawing and photograph of the same patient as figure 3 after nipple reconstruction and tattoo of the nipple-areolar complex.
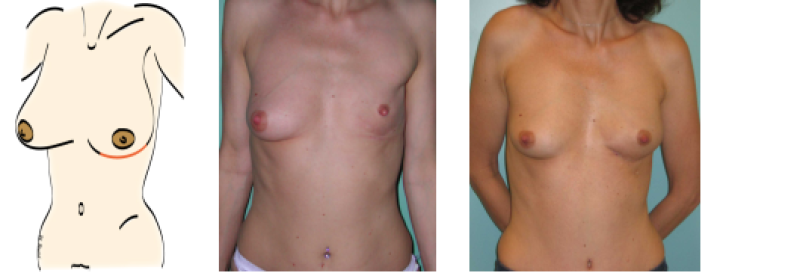
Figure above: schematic drawing and clinical example of a patient who underwent a subcutaneous mastectomy through an infra-mammary incision. She underwent a delayed autologous breast reconstruction through the same incision in a 2nd operative procedure.
References
Radical mastectomy. ATKINS H. Br J Surg. 1948 Jul;36(141):87-90.
Skin sparing mastectomy: anatomic and technical considerations. Carlson GW. Am Surg. 1996 Feb;62(2):151-5.
The value of skin-sparing mastectomy. Kroll SS. Ann Surg Oncol. 1998 Oct-Nov;5(7):660-2.
Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N. N Engl J Med. 2002 Aug 22;347(8):567-75.
The role of biological markers as predictors of response to preoperative chemotherapy in large primary breast cancer. Cocquyt VF, Schelfhout VR, Blondeel PN, Depypere HT, Daems KK, Serreyn RF, Praet MM, Van Belle SJ. Med Oncol. 2003;20(3):221-31.
Measuring quality of life in oncologic breast surgery: a systematic review of patient-reported outcome measures. Chen CM, Cano SJ, Klassen AF, King T, McCarthy C, Cordeiro PG, Morrow M, Pusic AL. Breast J. 2010 Nov-Dec;16(6):587-97.
Immediate conservative breast surgery reconstruction with perforator flaps: new challenges in the era of partial mastectomy reconstruction? Munhoz AM, Montag E, Arruda E, Brasil JA, Aldrighi JM, Gemperli R, Filassi JR, Ferreira MC. Breast. 2011 Jun;20(3):233-40.
What options for treatment of hereditary breast cancer? Narod S. Lancet. 2002 Apr 27;359(9316):1451-2.
Conservative mastectomies. Nava MB, Catanuto G, Pennati A, Garganese G, Spano A. Aesthetic Plast Surg. 2009 Sep;33(5):681-6.
What options for treatment of hereditary breast cancer? Narod S. Lancet. 2002 Apr 27;359(9316):1451-2.
Elston CW, Ellis IOPathological prognostic factors in breast cancer: the value of histological grade in breast cancer. Histopathology (1991) 19:403–410.
Sentinel node biopsy
During surgery for removal of a malignant breast tumor, it is also possible to evaluate the axillary lymph nodes for the presence or absence of loco-regional metastasis from the breast. The aim of this procedure is to determine the severity and extent of the disease. Based on the involvement of axillary nodes, additional (adjuvant) therapies will be arranged, including chemotherapy, radiotherapy, immunotherapy and / or hormonal therapy. If large or invasive tumors or multiple small invasive breast tumors are present, all the nodes in the lower part of the axilla are removed.
Previously, more aggressive surgery was undertaken i.e. removal of all the lymph nodes around the blood vessels and nerves of the arm and behind the clavicle (axillary clearance) but this appeared only to cause more complications without giving any additional information.
The major complications were lymphedema and chronic nerve pain in the arm. Lymphedema (inability to drain lymphatic fluid resulting in its accumulation in the affected limb) is still the most frequent complication of axillary surgery but is less frequent with more conservative measures. The risk of lymphedema is increased when radiation is administered to the axilla.
When the tumor is less than 2 cm, a sentinel node biopsy is performed. Before surgery, a mildly radioactive substance is injected around the tumor. This substance moves through the lymph vessels to the axillary nodes. The first axillary lymph node reached by the fluid, the sentinel node, is the most radioactive one (fig. 1). If malignant cells from the breast tumor pass into the lymphatic vessels then the sentinel node will be the first node involved.
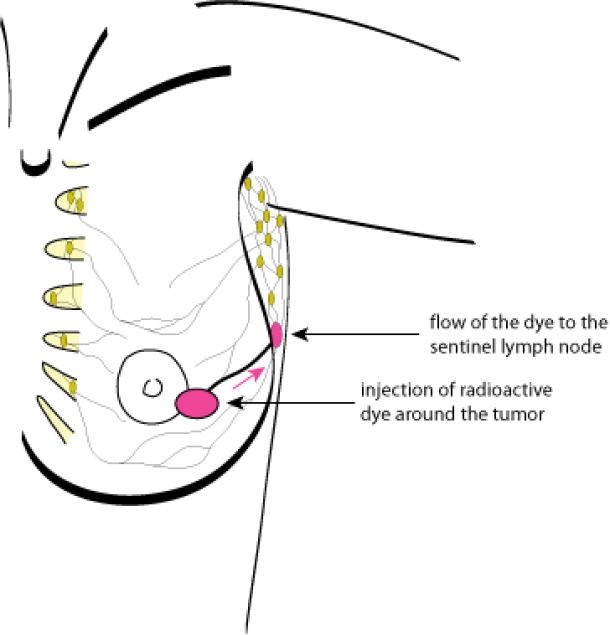
Figure 1: identification of the sentinel lymph node
During surgery, a sensitive device (Geiger counter) that measures radioactivity, is used to detect the sentinel node. This is then excised and sent for histological examination. If the sentinel node is free of malignant cells, it is not necessary to remove the other lymph nodes in the axilla. A sentinel node biopsy is a minimally invasive, short procedure. Side effects, including the risk of lymphedema, are minimal.
If the sentinel node is invaded by malignant cells, a conventional removal or “clearance” of the lower part of the axillary lymph nodes is performed in an additional surgical procedure (fig. 2).
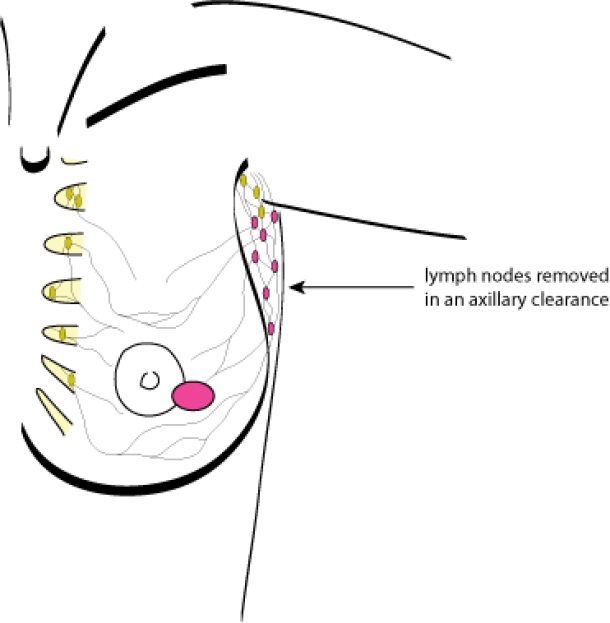
Figure 2: axillary lymph node removal
